In the realm of emergency medical services, EMT trauma patient assessment scenarios demand meticulous attention and swift action. This comprehensive guide delves into the intricacies of patient assessment, triage, stabilization, communication, documentation, and ethical considerations, equipping EMTs with the knowledge and skills to effectively manage trauma patients and optimize patient outcomes.
EMT trauma patient assessment scenarios require a systematic and thorough approach. Primary and secondary assessment methods provide a structured framework for evaluating patients, identifying injuries, and prioritizing care. Triage and stabilization techniques empower EMTs to prioritize patients based on the severity of their injuries and initiate life-saving interventions.
Effective communication and accurate documentation ensure seamless coordination among healthcare providers and facilitate optimal patient care.
Patient Assessment Procedures
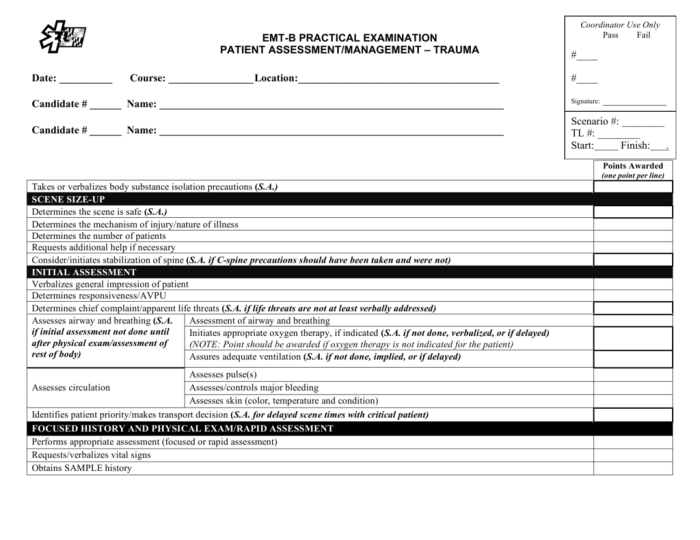
Thorough and accurate patient assessment is crucial in trauma situations to identify injuries, prioritize treatment, and ensure the best possible outcomes for patients. EMTs utilize two primary assessment methods: primary and secondary assessment.
Primary Assessment
- Airway assessment:Check for patency, obstruction, and adequacy of breathing.
- Breathing assessment:Assess rate, depth, and quality of breathing; listen for abnormal sounds.
- Circulation assessment:Evaluate pulse rate, quality, and capillary refill; check for bleeding.
- Disability assessment:Use the Glasgow Coma Scale (GCS) to assess level of consciousness and neurological function.
- Exposure assessment:Remove clothing to examine for injuries, wounds, and deformities.
Secondary Assessment, Emt trauma patient assessment scenarios
Once the primary assessment is complete, EMTs conduct a secondary assessment to gather more detailed information about the patient’s injuries and medical history.
- Head, neck, and spine assessment:Palpate for tenderness, deformity, or crepitus; check for neurological deficits.
- Chest assessment:Auscultate for breath sounds, assess for chest wall injuries, and check for pneumothorax or hemothorax.
- Abdominal assessment:Palpate for tenderness, rigidity, or distension; assess for organ damage.
- Pelvic assessment:Stabilize the pelvis, check for instability or deformity, and assess for rectal bleeding.
- Extremity assessment:Inspect for fractures, dislocations, or soft tissue injuries; assess pulses and capillary refill.
Triage and Stabilization
After assessing the patient, EMTs prioritize treatment based on the severity of injuries using a triage system. Common triage categories include:
- Priority 1:Life-threatening injuries requiring immediate intervention
- Priority 2:Serious injuries requiring prompt treatment
- Priority 3:Non-life-threatening injuries that can be managed later
- Priority 4:Minor injuries or no apparent injuries
Stabilization techniques are used to manage trauma patients and prevent further injury or deterioration. Common stabilization techniques include:
- Airway management:Establishing and maintaining a patent airway using suctioning, airway adjuncts, or intubation.
- Spinal immobilization:Immobilizing the head, neck, and spine to prevent further spinal cord injury.
- Wound care:Cleaning and dressing wounds to prevent infection and promote healing.
- Fracture stabilization:Splinting or casting fractures to prevent further displacement or damage.
- Fluid resuscitation:Administering fluids to maintain blood pressure and prevent hypovolemic shock.
Communication and Documentation: Emt Trauma Patient Assessment Scenarios
Effective communication between EMTs and other healthcare providers is essential for ensuring continuity of care and improving patient outcomes. EMTs must clearly and accurately communicate patient assessments, treatments, and any relevant information to receiving facilities.
Documentation is crucial for maintaining a record of patient care and ensuring accountability. EMTs must accurately document all patient assessments, treatments, and medications administered. Documentation should include:
- Patient demographics and vital signs
- Assessment findings
- Treatments provided
- Time and date of interventions
- Signatures of all healthcare providers involved
Ethical Considerations
EMTs face ethical considerations when caring for trauma patients. The principles of patient autonomy, beneficence, and non-maleficence guide their decision-making.
- Patient autonomy:Respecting the patient’s right to make informed decisions about their care, even in emergency situations.
- Beneficence:Acting in the patient’s best interests, providing care that is intended to benefit them.
- Non-maleficence:Avoiding harm to the patient, prioritizing their safety and well-being.
Balancing these principles can be challenging in trauma situations. EMTs must consider the patient’s wishes, their medical condition, and the potential consequences of their actions to make ethical decisions that prioritize the patient’s well-being.
Essential FAQs
What are the key principles of ethical considerations in EMT trauma patient assessment?
Patient autonomy, beneficence (doing good), and non-maleficence (avoiding harm) are the guiding principles for EMTs in trauma care.
How does triage help EMTs prioritize trauma patients?
Triage involves rapidly assessing patients to determine the severity of their injuries and allocate resources accordingly, prioritizing those with life-threatening injuries.
What are some common stabilization techniques used by EMTs for trauma patients?
Stabilization techniques include controlling bleeding, splinting fractures, managing airway and breathing, and administering pain medication.
Why is effective communication crucial in EMT trauma patient assessment scenarios?
Clear and concise communication ensures accurate patient information sharing among EMTs and other healthcare providers, facilitating timely and appropriate interventions.